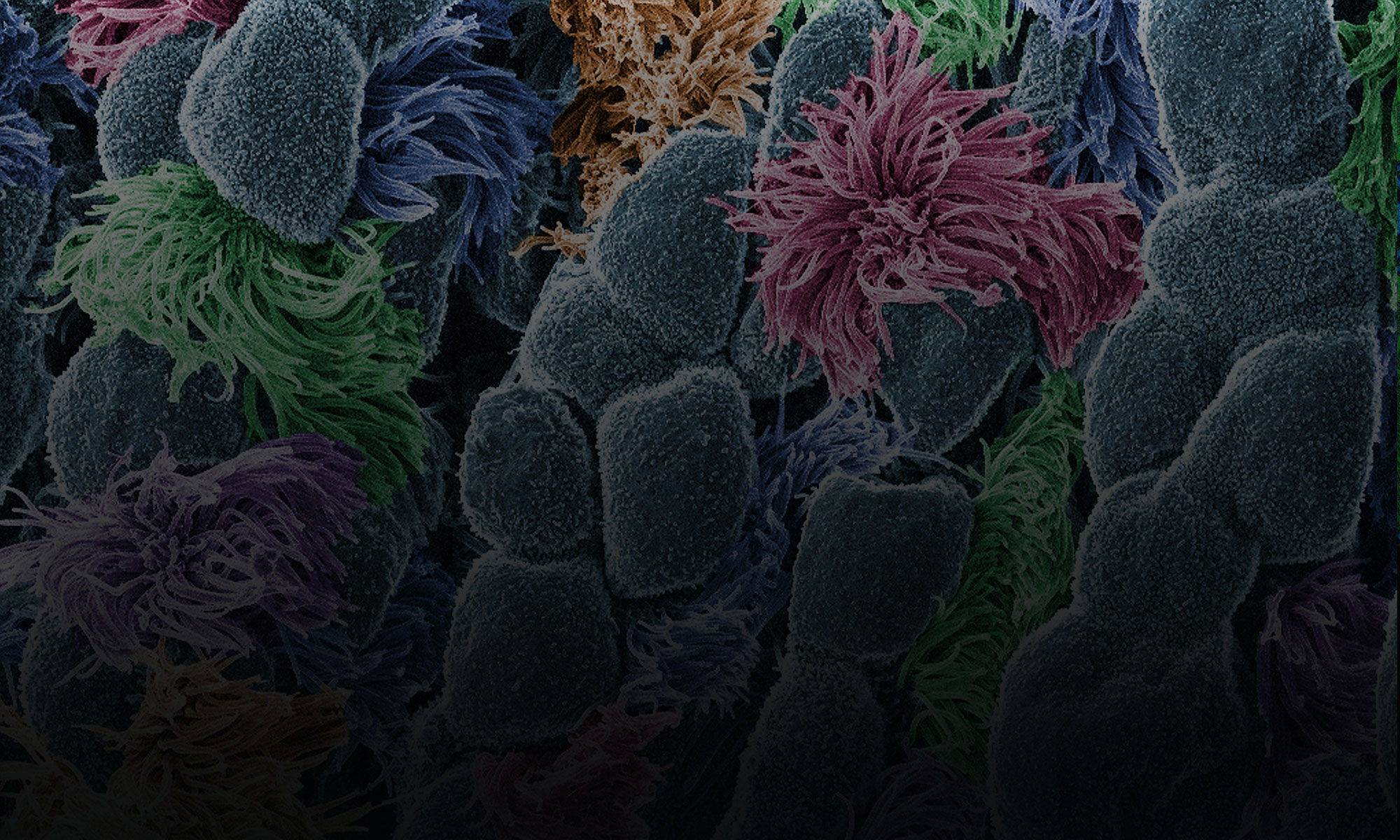
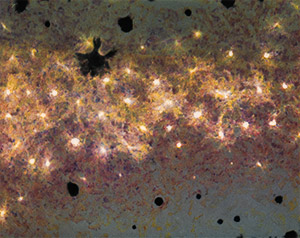
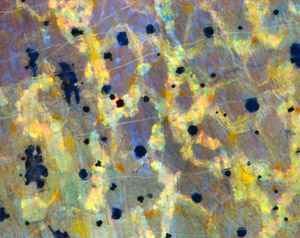
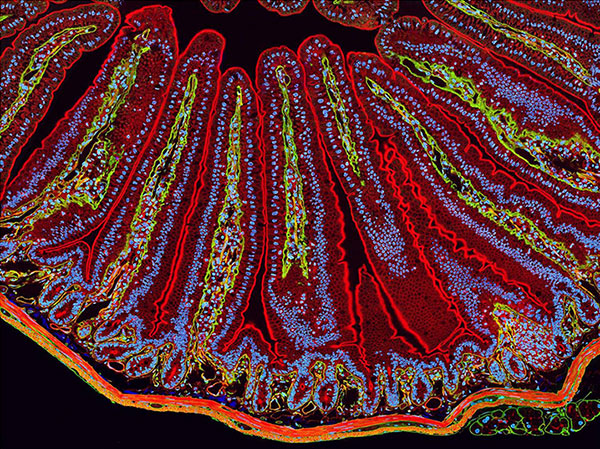
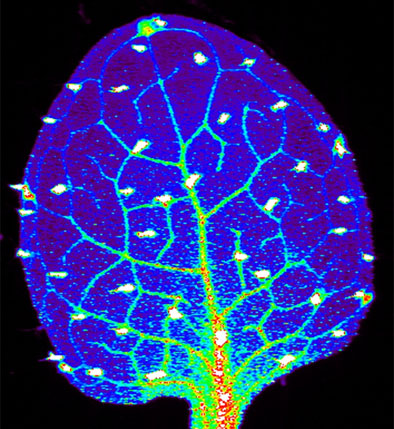
Science is beautiful.
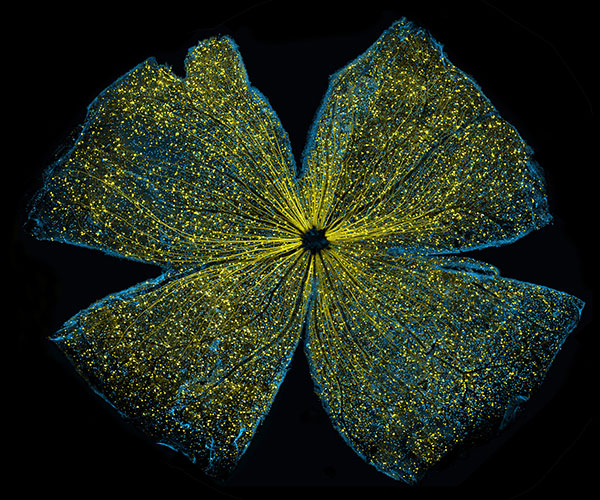
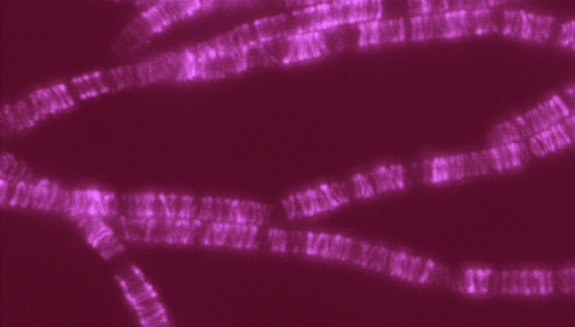
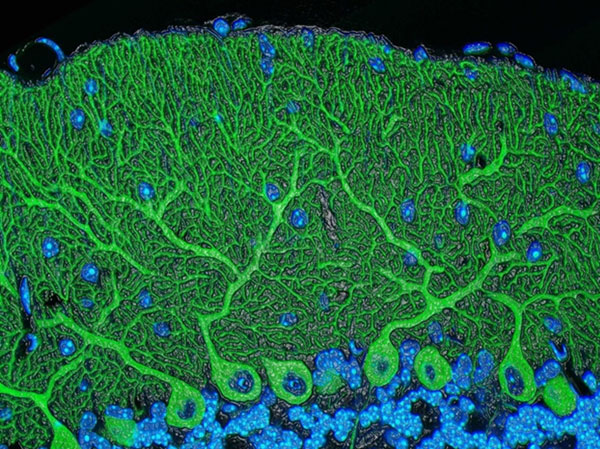
For several years, we’ve used this blog to highlight pictures we think are cool, scientifically relevant and visually striking. The images were created by NIGMS-funded researchers in the process of doing their research. Many come from our Life: Magnified collection, which features dozens of stunning photos of life, close-up. We’ll continue to bring you interesting images and information here on Biomedical Beat, but if you can’t get enough of them, we have a new way to share our visual content with you: Instagram.
We’re pleased to announce the launch of our NIGMS Instagram account. We’ll highlight gorgeous images, and bring you the science behind them—straight from our mobile device to yours. Instagram lets us label our images with subject-specific hashtags. You can find our pictures by going on Instagram and searching for #NIGMS. If you’re already an Instagram user, you can follow us @NIGMS_NIH. You can even see our page using a web browser at https://www.instagram.com/nigms_nih/ ![]() . Let us know what you think!
. Let us know what you think!
Also, if you have any stunning images or videos that relate to scientific areas supported by NIGMS, please send them to us. They might end up on our Instagram feed!
#science
#science
#science

#biology