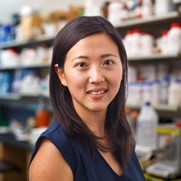
“I think there’s a very creative side to science, in figuring out how to approach a problem, which I find really engaging,” says Mia Huang, Ph.D., an associate professor of chemistry at the Scripps Research Institute in La Jolla, California. In an interview, Dr. Huang discussed her shift in interest from medicine to science, her graduate school work on nature-inspired antifreeze molecules, and her lab’s exploration of the roles of sugar-coated proteins in our bodies.
Get to Know Dr. Huang
- Coffee or tea? Coffee
- Favorite music genre? EDM
- Cats or dogs? Dogs—I’m a proud mom to a 15-pound Bernedoodle
- Rainy or sunny? Sunny
- What was your childhood dream job? Scientist—I’m living the dream!
- Favorite hobby? Playing video games
- Favorite piece of lab safety equipment? Safety goggles
- A scientist (past or present) you’d like to meet? Gilbert Ashwell and Anatol Morell (accidentally co-discovered the asialoglycoprotein receptor)
Continue reading “Where the Sugars and the Proteins Play: Q&A With Mia Huang”