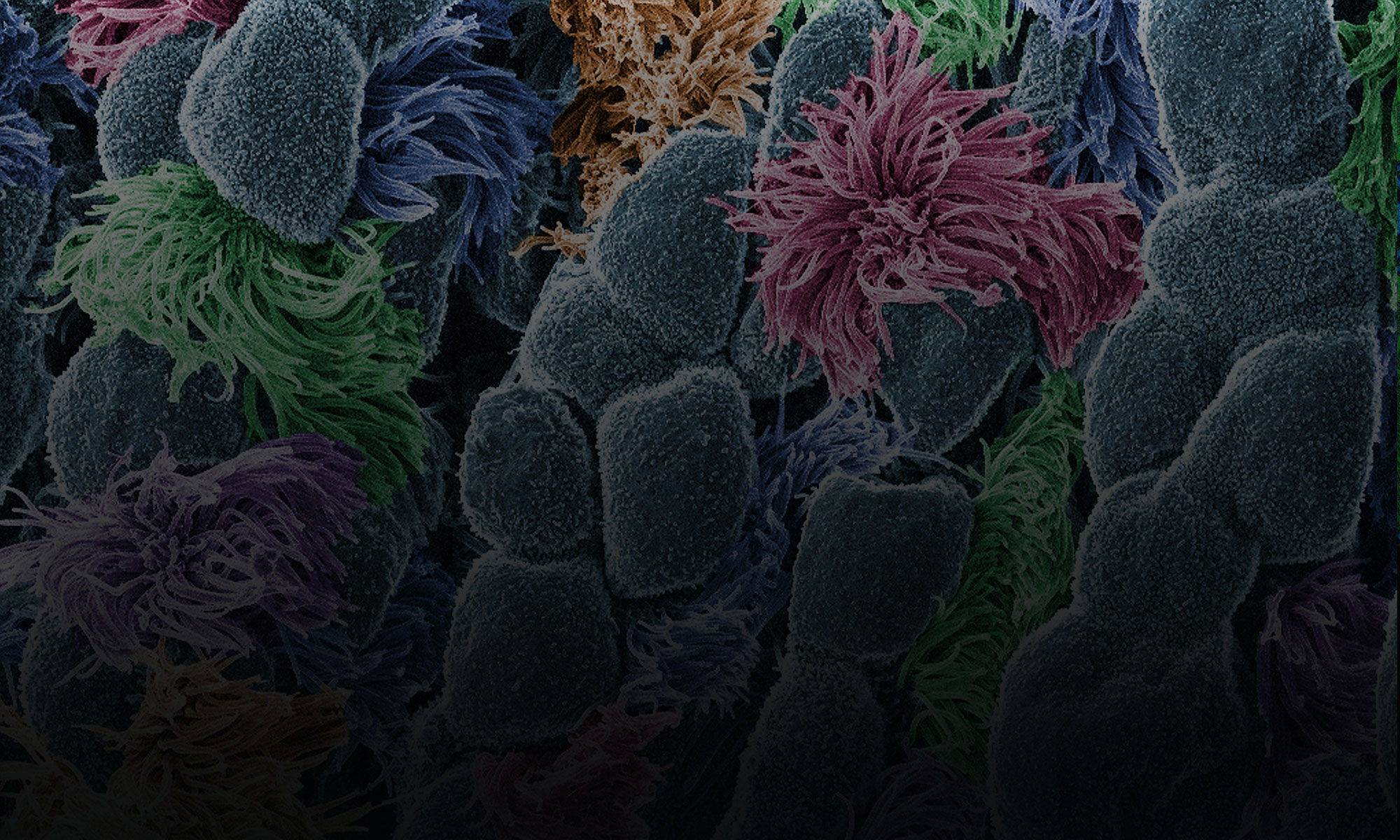
Sepsis is a serious medical condition caused by an overwhelming immune response to infection. The body’s infection-fighting chemicals trigger widespread inflammation, which can lead to blood clots and leaky blood vessels. As a result, blood flow is impaired, depriving organs of nutrients and oxygen. In severe cases, one or more organs fail. In the worst cases, blood pressure drops, the heart weakens, and the patient spirals toward septic shock. Once this happens, multiple organs—lungs, kidneys, liver—may quickly fail, and the patient can die.
Because sepsis is traditionally hard to diagnose, doctors do not always recognize the condition in its early stages. In the past, it has been unclear how quickly sepsis needs to be diagnosed and treated to provide patients with the best chance of surviving.

Now we may have an answer: A large-scale clinical study, published recently in the New England Journal of Medicine, found that for every hour treatment is delayed, the odds of a patient’s survival are reduced by 4 percent. Christopher Seymour, assistant professor of critical care and emergency medicine at the University of Pittsburgh, and his team analyzed the medical records of nearly 50,000 sepsis patients at 149 clinical centers to determine whether administering the standard sepsis treatment—antibiotics and intravenously administered fluids—sooner would save more lives.
I spoke with Seymour about his experience treating sepsis patients and his research on the condition, including the new study.
CP: How big a public health problem is sepsis?
CS: Our recent work with the Centers for Disease Control and Prevention suggests there might be as many as 2 million sepsis cases in the United States each year. I can share personally that sepsis, or septic shock, is far and away the most common life-threatening condition that I treat in the ICU (intensive care unit). It’s quite devastating, particularly among our elders, and it requires prompt care. Although the mortality rate may be decreasing, it’s still quite high. About 1 in 10 patients with sepsis don’t survive their hospital stay. Even young, healthy people can succumb from sepsis. And if you’re fortunate to survive, you can have significant problems with cognitive and physical function for many months to years down the line.
Unfortunately, the incidence of sepsis may even be increasing. More patients are surviving serious illnesses that used to be fatal. They’re alive, but their health is compromised, so they are at higher risk for sepsis. Also—and this is a positive—we are seeing greater recognition and increased reporting of sepsis. Both factors probably contribute to the higher numbers of reported sepsis cases.
CP: What are some of the biggest challenges in fighting sepsis?
CS: The first challenge is public awareness. It’s important that the public knows the word sepsis, that they’re familiar with sepsis being a life-threatening condition that results from an infection, and that they know it can strike anyone—young, old, healthy, or sick. But it’s also important to know that not every infection is septic, nor will every cut or abrasion lead to life-threatening organ dysfunction.
Another part of the problem is that sepsis is not as easy for patients to recognize as, say, myocardial infarction (heart attack). When patients clutch their chest in pain, they intuitively recognize what’s happening. Patients frequently don’t recognize that they’re septic. People should know that when they have an infection or take antibiotics as an outpatient, and they’re starting to feel worse or having other new symptoms, they may be at risk of sepsis. They should go to the emergency department or seek medical help.
The second challenge in fighting sepsis is that it’s just hard to diagnose, even for well-trained clinicians. Both issues can lead to delays in care, the most important of which is the delay in treatment with antibiotics.
CP: Tell me about your recent clinical trial. What question did you set out to answer?
CS: There’s been a lot of interest in the early recognition and treatment of sepsis over the past decade. Recently, the National Institutes of Health/National Institute of General Medical Sciences funded a large, multicenter trial called ProCESS, which tested various strategies for treating sepsis. This trial told us that a standardized sepsis protocol among people who had already received antibiotics didn’t necessarily change survival rates. But what it left unanswered was the very important question of when the patient first arrives at the emergency department, how fast do we need to provide antibiotics and fluids for the best possible outcome?
That’s what we wanted to learn. We worked with colleagues in New York state, which recently mandated a standardized treatment protocol for patients who were diagnosed as septic within their first 6 hours in the emergency department. Specifically, we asked, will these patients have a better chance of survival if we deliver care within 3 hours of their sepsis diagnosis?
CP: And what did you find?
CS: Essentially, time mattered. The faster the patients received treatment, the more likely they were to survive. And that was the case even for this group of patients, who had already been diagnosed relatively early—within 6 hours of entering the hospital.
The study revealed that if treatment was completed in, for example, 3 hours, patients had a 4 percent reduction in the odds of in-hospital mortality than if it was completed in 4 hours. And that takes into account other risk factors such as age, site of infection, and the presence of shock.
Our results were corroborated by a team led by our colleague Vincent Liu in California. He and his team recently published an independent study of 30,000 Kaiser Permanente Northern California patients. Their study also showed that every hour in delaying treatment led to significantly increased mortality, particularly in the sickest patients.
CP: How do you anticipate these findings will influence medical professionals?
CS: As clinicians first evaluate sick patients, we hope that sepsis is at the forefront of their minds. The increasing public health burden of sepsis and the high mortality suggest that physicians and other caregivers should be thinking about this condition all the time. The specific take-home message from our study is that timing matters, and they should be ordering the appropriate blood tests, looking for organ dysfunction, and administering antibiotics as soon as possible.
There’s also potential policy implications. Regulations in New York, Illinois, and a few other states regarding sepsis have already been implemented. We would hope that these regulations continue to encourage hospitals and clinicians to treat septic patients early but also allow for flexibility in the face of new research findings. One potential downside of standardizing care is that it may be hard to update the protocols in response to new data.
CP: What’s next for your team?
CS: We will continue our research to identify clinical or biologic signatures (such as accelerated heart rate or elevated levels of a specific protein in the blood) to provide more precise, earlier treatment with newer therapeutics. We also want to find ways to identify patients who don’t respond to traditional treatments so we can give them alternate therapies in a timely way. Taken together, we hope to save more lives from sepsis.
Christopher Seymour’s research is funded in part by NIGMS under grant R35GM119519.
Excellent Q&A
I went to the emergency room by ambulance as I could not walk….my leg was swollen severely and the pain was excruciating. The doctor in the er didn’t even look at my leg didn’t do any blood work. Said I was fine gave ne 3 hydrmorphin pills and sent me home. We were floored. I layed on my couch for nine days like that
Luckily I had a Dr appointment nine days later which I hardly remember my husband said they took fluid off my knee that he said looked like soap. That same night they called and said to go to the hospital I had surgery to flush the septic and had my meniscus removec. I was in hospital for 6 days. and had a pic line in for 2 months Then weeks layer we received a strange letter from a head Dr The letter had nothing to do with why I was at the er.It was actually insulting. He said that I really shouldn’t have gone to the er. Then when I went to see my family Dr. he told me the er Dr called him to apologize. It was an awful experience and I have not felt right since.My anxiety level is horrible! I can’t believe this happened!