
Spike proteins on the surface of a coronavirus. Credit: David Veesler, University of Washington.
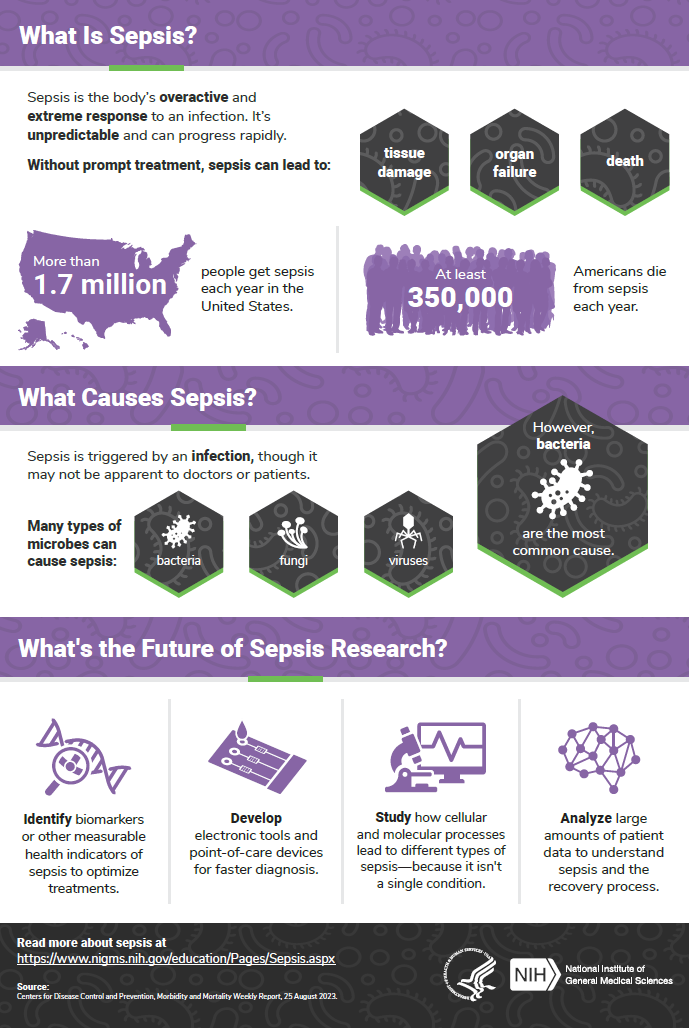
Since the start of the COVID-19 pandemic, researchers from many areas of biomedical science have worked together to learn how this new disease affects the human body, how to prevent its spread, and how to treat it. Severe cases of COVID-19 and cases of sepsis share many symptoms. Sepsis is the body’s overactive and extreme response to an infection. It’s unpredictable and can progress rapidly. Without prompt treatment, it can lead to tissue damage, organ failure, and death.
Sepsis has similarities with some cases of COVID-19, most likely because the two conditions trigger the same reactions at the cellular level. Researchers have studied these reactions in sepsis for many years.
“When we look back on 2020 and the speed with which progress was made against COVID-19, two features will stand out,” says John Younger, M.D., a member of the NIGMS Advisory Council who recently co-chaired a working group on advancing sepsis research. “The first is how quickly the biotechnology community came together to develop vaccine candidates. The second, and arguably the most immediately impactful, is how caregivers and clinical researchers were able to rapidly refine the care of COVID-19 patients based on decades of experience with sepsis.”
This post highlights a few of the many sepsis researchers supported by NIGMS who are applying their expertise to COVID-19.
Continue reading “Fight Against COVID-19 Aided by Sepsis Researchers”







 Dr. Darden with her mentor, Dr. Philip Efron. Credit: Courtesy of Lyle Moldawer, Ph.D.
Dr. Darden with her mentor, Dr. Philip Efron. Credit: Courtesy of Lyle Moldawer, Ph.D.
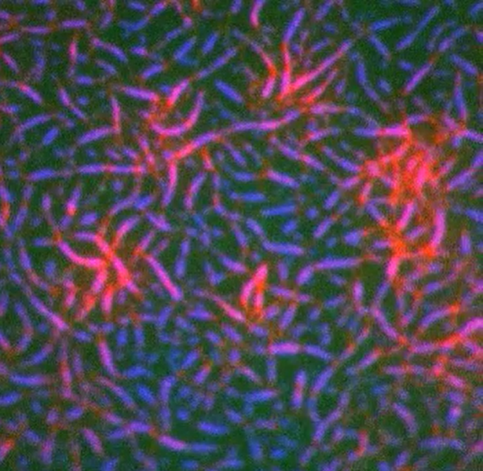
 Spike proteins on the surface of a coronavirus. Credit: David Veesler, University of Washington.
Spike proteins on the surface of a coronavirus. Credit: David Veesler, University of Washington.