
“I find it fulfilling to be a scientist because I know that even if at some points it seems like I’m working on an incremental experiment, eventually it’s going to help solve a bigger problem,” says Caroline Jones, Ph.D., an assistant professor of bioengineering at the University of Texas at Dallas. Check out the highlights of our interview with Dr. Jones to learn about her career path, her passion for sharing science with the public, and her research on sepsis—an overwhelming or impaired whole-body immune response to an insult, such as an infection or injury that’s responsible for the deaths of nearly 270,000 Americans every year.
Q: How did you first become interested in science?
A: My mother was a high school math teacher, so I had that role model growing up. I also had a math and engineering teacher in high school who encouraged me and sparked my interest in the quantitative side of science. I decided to study biomedical engineering in college because I wanted to apply quantitative tools in a way that helped people.
Q: What was your path to becoming a researcher?
A: My first research experience was when I was an undergrad at Cornell University in the lab of Dr. Peter Nathanielsz. I was really inspired by his research on pregnancy and newborn health. He was my first mentor, and he instilled in me the importance of communicating your science. He would give lectures at the local library, and he wrote books for the general public.
After undergrad, I earned a master’s degree at Cornell, where I worked on detecting pathogens using liposomes in the lab of Dr. Antje Baeumner. From there, I wasn’t quite sure if I wanted to pursue a Ph.D., so I moved to New York City and worked as a lab technician at Rockefeller University with Drs. Markus and Archontoula Stoffel. I became involved in an interesting genome-wide association study in an isolated population from the Pacific Island of Kosrae.
Deciding that I did want to pursue a Ph.D. in biomedical engineering, I moved across the country to do my research in the lab of Dr. Alexander Revzin at the University of California, Davis. I studied how the function of liver cells is impacted by the microenvironment around them.
Q: What were the next steps in your career?
A: I took a postdoctoral position at the Center for Engineering in Medicine and Surgery at Massachusetts General Hospital. That was the first time that NIGMS impacted me, because I was on a T32 training grant with Dr. Ronald Tompkins. I developed microfluidic tools to measure how burns affect immune cells under the mentorship of Dr. Mehmet Toner, Dr. Daniel Irimia, and Octavio Hurtado. That was really where I found my passion for translational research, through using engineering and mathematical techniques but also working with samples from patients with sepsis, and I knew that this type of research would impact human lives.
We saw that immune cells behaved differently in patients with burns who went on to develop sepsis versus those who had a normal inflammatory response to the burn. We made a tool to predict whether patients would develop sepsis, which is a huge question in the field because if it isn’t diagnosed early enough, it can lead to organ failure and death. We have a patent on the tool now, which was 98 percent accurate in our experiments, and it’s undergoing further testing.
After 5 years as a postdoc, I got my first faculty position at Virginia Tech as an assistant professor of immunology. During my 5 years there, I received my first independent research funding from NIGMS, the Maximizing Investigators’ Research Award, and then I moved to the University of Texas at Dallas as an assistant professor in bioengineering.
Q: What do you research in your lab?
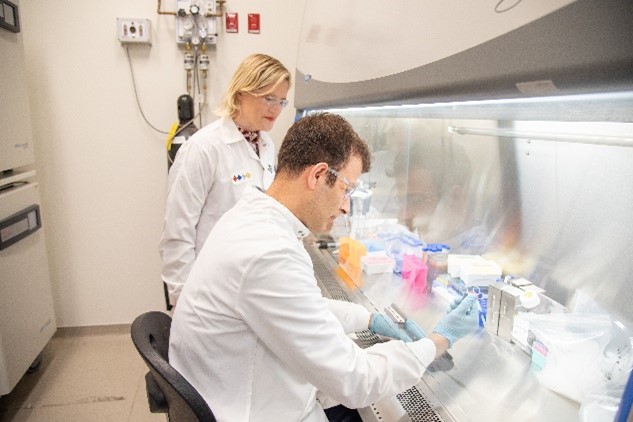
A: My lab develops tools to measure immune cell function in septic patients. Basically, we build chips with small channels that range from about the size of a hair to even smaller than a cell. Then, we create gradients or specific signals to attract the cells and measure how they migrate and how they fight infection. We take time-lapse movies of the cells migrating so we can collect data about their phenotypes—or their characteristics and behavior. Then we connect the cells’ phenotypes to their genotypes—collections of genes—by retrieving the cells off the chip and sequencing their mRNA expression levels. We collaborate with mathematicians to make models of how changes in receptor or certain protein levels will change cell migration. This enables us to identify and predict the mechanisms that cause specific phenotypes. We hope that by recognizing mechanisms that underlie sepsis, we will ultimately find treatments that target those mechanisms and help treat the condition. It’s an exciting time to be an immunoengineer!
Q: What do you consider your biggest achievement so far?
A: Leading a successful interdisciplinary team that speaks so many different scientific languages to work on the huge challenge of sepsis has been one of my biggest achievements. The team includes biomaterials scientists, mechanical engineers, mathematicians, immunologists, and physicians.

Q: You mentioned the importance of communicating your science to the public. How do you do this?
A: I’ve given lectures through the Dallas Public Library, and that’s been really fulfilling because I can communicate about sepsis, vaccines, or COVID-19, and people can ask questions. It’s very important to gain public trust in scientific research. The public is funding my work, so I want to give back to them. The more I talk to them, the more I realize how many are personally impacted by sepsis. My own great-grandmother, Edith Jones, died of it when she was pregnant at age 39. It’s my goal to create more awareness around sepsis and make an impact with my own research to reduce resulting deaths.
Also, because of my love for creativity and art, I’ve worked with artists to make a virtual reality game where you can be an immune cell. Right now, it’s in the preliminary stages. We published a couple of manuscripts on it, and we’re taking it to lower-income high school classes and testing it. Communicating through images or experiences can be very powerful. Through this outreach, I hope to recruit more women and underrepresented students to pursue careers in science and engineering.
Q: What advice do you have for students interested in pursuing a career in science?
A: If at all possible, reach out to a laboratory and get hands-on experience working there. To gain a lot of scientific skill sets, you really need to work in a lab but also have things outside of the lab that inspire you. Reading a novel, watching a good movie, or painting a picture takes time away from work, but having a life outside of the lab fills the well of your creativity so that you’re a better scientist at the end of the day.
Dr. Jones’ research is supported by NIGMS grant R35GM133610.


