The immune system is designed to closely monitor the body for signs of intruders that may cause infection. But what happens if it malfunctions? Overactive and underactive immune systems can both have negative effects on your health.
Autoimmune Disorders
To effectively monitor the body for pathogens, the adaptive immune system has to learn what a pathogen “looks like” on a molecular level. During their development, white blood cells go through training to learn how to differentiate “self” from “non-self.” They are trained to avoid attacking any “self” cells, which includes all types of human cells.
Sometimes this training fails, creating white blood cells that target “self” and cause autoimmune disorders. For example, type 1 diabetes results when the immune system wrongly attacks the pancreas, which is the organ that produces insulin—a hormone that controls blood sugar levels. People with type 1 diabetes must take insulin injections to keep their blood sugar within a safe range.
Immunodeficiency Disorders
Sometimes the immune system doesn’t work effectively to prevent infections. Doctors and researchers call this immunodeficiency. Immunodeficiency disorders can involve any cell type of the immune system and can be either inherited (genetic) or acquired (caused by external factors).
X-linked agammaglobulinemia (XLA) is an example of an inherited immunodeficiency disorder. People with XLA make very few white blood cells called B-cells, which are a type of adaptive immune cell. They therefore can’t generate antibodies effectively and are thus highly susceptible to infection and unresponsive to vaccination.
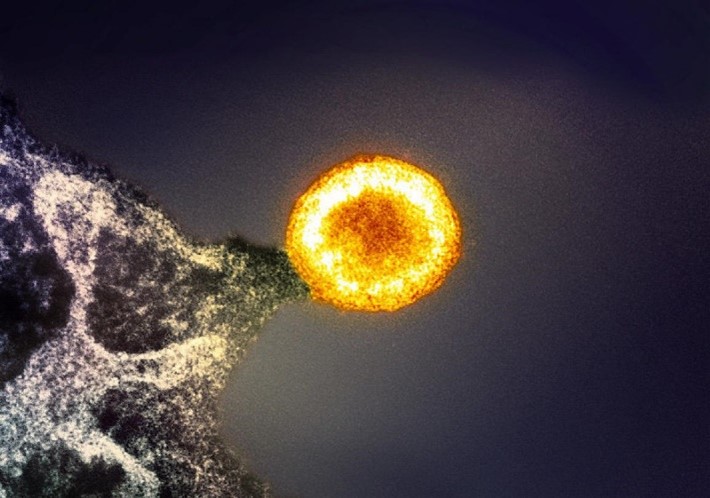
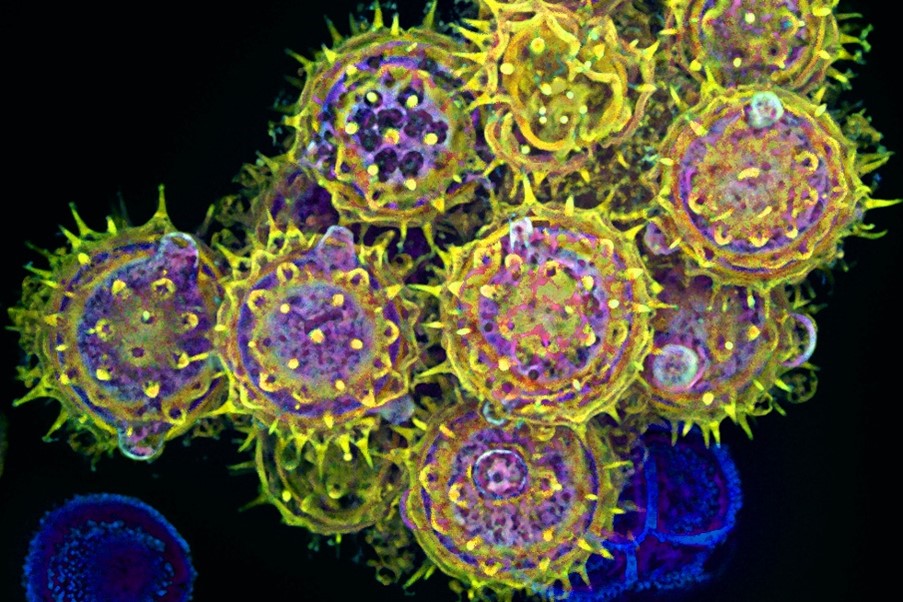
On the other hand, infection by the human immunodeficiency virus (HIV) can cause a form of acquired immunodeficiency. HIV infects and kills white blood cells called T-cells. Uncontrolled HIV infection may lead to acquired immunodeficiency syndrome (AIDS), which is associated with frequent infections by bacteria, fungi, or other viruses.
Sepsis
Sepsis is a condition that occurs when a person’s immune system responds improperly to certain insults, such as bacterial, viral, or fungal infections or other injuries. Under normal conditions, the immune system releases chemical or protein mediators into the blood to combat the infection or injury. If uncontrolled, those mediators can trigger widespread inflammation that impairs blood flow to organs, depriving them of nutrients and oxygen and leading to organ damage.
At least 1.7 million adults in the United States develop this life-threatening condition each year. Those at highest risk of developing sepsis are infants, children, older adults, and those with underlying medical conditions such as diabetes, cancer, or liver disease.
Allergies
When white blood cells get trained to recognize “self” from “non-self,” they also get trained to distinguish harmful from harmless “non-self.” When this part of the training fails, people may develop an allergy—a reaction to a harmless substance that doesn’t affect most other people.
People can develop allergies to many substances, called allergens, including:
- Dust mites
- Food
- Insect stings
- Medicines
- Mold spores
- Pet dander
- Pollen
Allergies cause a range of symptoms, depending on the allergen and the severity of the allergy. These symptoms can include a runny nose, sneezing, itching, and rashes. Severe allergies may cause anaphylaxis, a life-threatening reaction that can trigger swelling of the lips and tongue and difficulty breathing.
The serious effects of an immune system gone awry underscore what an important role this trained network plays in our well-being.
Find the teaching activity that corresponds with this post in our Educator’s Corner.