What Is Computer Modeling and How Does It Work?
Recent news headlines are awash in references to “modeling the spread” and “flattening the curve.” You may have wondered what exactly this means and how it applies to the COVID-19 pandemic. Infectious disease modeling is part of the larger field of computer modeling. This type of research uses computers to simulate and study the behavior of complex systems using mathematics, physics, and computer science. Each model contains many variables that characterize the system being studied. Simulation is done by adjusting each of the variables, alone or in combination, to see how the changes affect the outcomes. Computer modeling is used in a wide array of applications, from weather forecasting, airplane flight simulation, and drug development to infectious disease spread and containment.
In weather forecasting, for example, models are built by feeding data such as pressure, wind, temperature, and moisture into mathematical equations to predict what may happen in the future. For any given weather projection, there are many different models created that use various mathematical equations. Sometimes the models closely align with each other while other times they disagree. In either case, they need to be interpreted by an expert to provide a reliable, though not perfect, forecast. While it would be ideal to have a single model applicable to all scenarios, we have yet to develop one. Each model is complex and has strengths and weaknesses for a given scenario based on the mathematical formulas that were used and the availability and quality of relevant data.
How Do Models Help Forecast the Spread of Infectious Diseases?
In a similar fashion, multiple models exist for forecasting the spread of infectious diseases. These models use existing data related to disease transmission, symptoms and health complications, and other factors to estimate the number of people who will become infected and, in some cases, die from the disease. This helps public health professionals predict needs for critical supplies, such as clinical staff, hospital beds, and protective equipment. Developing such models becomes more complicated when data is inaccessible, unavailable, or incomplete, particularly in the case of a completely new infectious agent such as COVID-19. The effects of interventions to lessen the impact of the disease, such as access to supportive care, stringent containment measures, timely response, restriction of mobility, and diagnostic and therapeutic resources, can also be incorporated into the models. More information about mitigation strategies can be found in the Centers for Disease Control’s Community Mitigation Guidelines to Prevent Pandemic Influenza — United States, 2017.
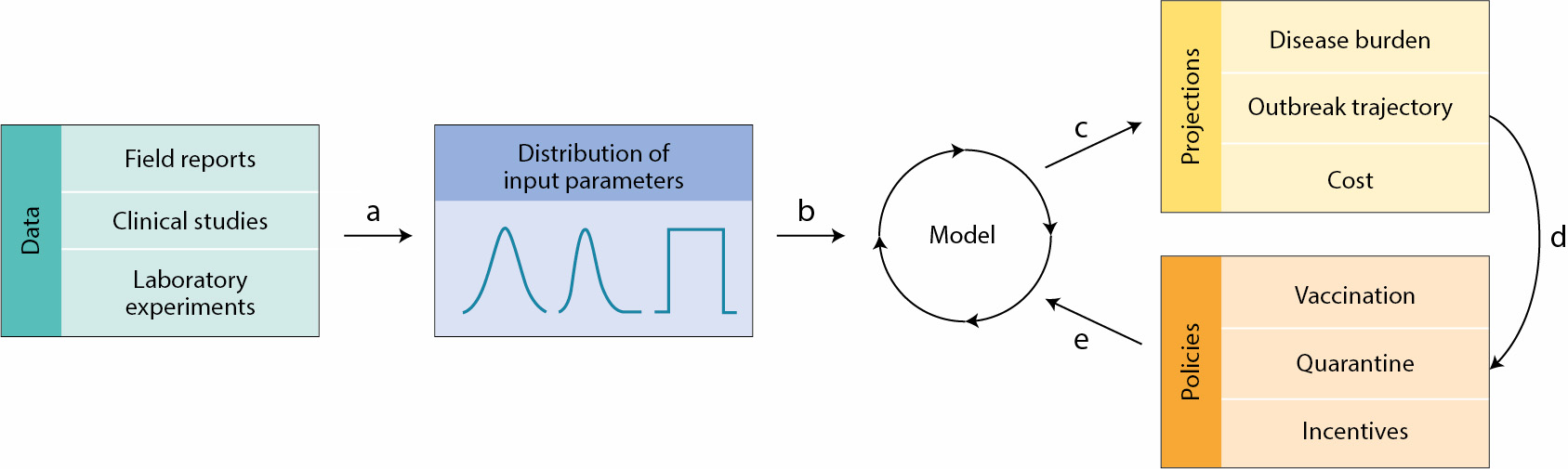 Multiple data sources are used in conjunction with different scenarios for spread within the community to create models, leading to projections of factors such as the path of the outbreak, disease burden, and cost. As policies are adopted and the real-life situation changes, the model can be updated over and over again, thus optimizing policies. Credit: Reprinted by permission from Springer Nature: Nature Microbiology. Modelling microbial infection to address global health challenges, Meagan C. Fitzpatrick et al., 2019. Click to enlarge
Multiple data sources are used in conjunction with different scenarios for spread within the community to create models, leading to projections of factors such as the path of the outbreak, disease burden, and cost. As policies are adopted and the real-life situation changes, the model can be updated over and over again, thus optimizing policies. Credit: Reprinted by permission from Springer Nature: Nature Microbiology. Modelling microbial infection to address global health challenges, Meagan C. Fitzpatrick et al., 2019. Click to enlarge
Given incomplete knowledge or a gap in historical data and information, modeling can give decision-makers some level of justification for taking certain steps to mitigate risk to the general public. It is important, however, to avoid overinterpreting models. For example, in the early stages of an outbreak with very limited data, models often predict large impacts, but the reality turns out to be less dire. This phenomenon is illustrated in the pandemic influenza model below. Rather than indicating that the model was wrong, this often means that interventions had the intended effect. Continually feeding models with updated and accurate data is essential to improving their accuracy and thus their usefulness.
 The graph shows the potential effects of mitigation strategies on pandemic influenza. Click to enlarge
The graph shows the potential effects of mitigation strategies on pandemic influenza. Click to enlarge
What Is NIGMS Doing to Support Computer Modeling Research?
NIGMS funds the research of many individual scientists who are using computer modeling to understand how infectious diseases spread and to develop improved methods for detecting and mitigating infectious disease threats. In addition, the Institute supports the Models of Infectious Disease Agent Study (MIDAS) coordinating center, based at the University of Pittsburgh’s Graduate School of Public Health. The center is tasked with facilitating and coordinating infectious disease modeling research. It provides researchers in the MIDAS Network with access to datasets, experimental models, algorithms, computer code, and model parameters. It also supports cloud-computing resources for infectious disease modeling research. In addition, the center promotes the training of the next generation of infectious disease modeling researchers and maintains communication between public health agencies and the modeling research community. The goal of all of this work is to accelerate the rate of discoveries and innovation for the detection and control of infectious diseases. The MIDAS Network currently has more than 300 members, and any infectious disease scientist, practitioner, or student can request to join the network and get access to the coordinating center’s information and resources. Many of the network members are conducting research on COVID-19 and are contributing to an extraordinary international collection of data and information regarding the outbreak. In response to the COVID-19 pandemic, the coordinating center created a central online repository for the scientific community—a clearinghouse for sharing data and data-driven discoveries about COVID-19. The more we’re able to openly share insights, data, and resources, the better positioned we’ll be to respond to this and future disease outbreaks.
Now Watch This: PBS NewsHour Student Reporting Labs Interview with Wilbert Van Panhuis
Professor and epidemiologist Wilbert Van Panhuis, M.D., Ph.D., from the MIDAS National Center of Excellence, University of Pittsburgh, discusses how he’s collecting data on COVID-19.


I refer the author to:
“Exploratory Data Analysis”
By John W. Tukey.
I could go off on “Modeling” and “Simulations”, and of course “Emulation”, but I feel that would be in vain.