“It’s a thrill to make a discovery in science. In that moment, you’re the only one who knows about this new finding. Then you get to share that discovery with the world,” says Chelsey Spriggs, Ph.D. Dr. Spriggs is an assistant professor of cell and developmental biology at the University of Michigan (UMich) in Ann Arbor. We spoke with Dr. Spriggs about her early introduction to science through school science fairs, current research on viruses, and efforts to broaden participation in microbiology research across the world.
Get to Know Dr. Spriggs
- Books or movies? Books
- Coffee or tea? Coffee
- Favorite music genre? R&B (’90s and ’00s)
- Cats or dogs? Guinea pigs
- Early bird or night owl? Early bird
- Childhood dream job? Veterinarian
- Favorite hobby? Painting
- Favorite pipette size? 200uL
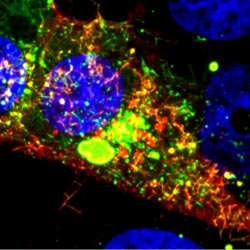
- Favorite lab tool? Confocal microscope



 Dr. Idhaliz Flores-Caldera.
Dr. Idhaliz Flores-Caldera.