Women have two X chromosomes (XX) and men have one X and one Y (XY), right? Not always, as you’ll learn from the quiz below. Men can be XX and women can be XY. And many other combinations of X and Y are possible.
Continue reading “Chromosomally speaking, what do you know about sex? Take a quiz to find out.”Pathways: New Scholastic Resources on Basic Science and Career Paths
 Cover of Pathways student magazine.
Cover of Pathways student magazine.
NIGMS and Scholastic, Inc., have collaborated to bring you Pathways, a collection of free resources that teaches students about basic science, its importance to human health, and research careers that students can pursue.
Continue reading “Pathways: New Scholastic Resources on Basic Science and Career Paths”Five Fabulous Fats
Happy Fat Tuesday!
On this day, celebrated in many countries with lavish parties and high-fat foods, we’re recognizing the importance of fats in the body.
You’ve probably heard about different types of fat, such as saturated, trans, monounsaturated, omega-3, and omega-6. But fats aren’t just ingredients in food. Along with similar molecules, they fall under the broad term lipids and serve critical roles in the body. Lipids protect your vital organs. They help cells communicate. They launch chemical reactions needed for growth, immune function, and reproduction. They serve as the building blocks of your sex hormones (estrogen and testosterone).
Here we feature five of the hundreds of lipids that are essential to health.
Continue reading “Five Fabulous Fats”Roses Are Red and So Is . . . Blood?
When you think of blood, chances are you think of the color red. But blood actually comes in a variety of colors, including red, blue, green, and purple. This rainbow of colors can be traced to the protein molecules that carry oxygen in the blood. Different proteins produce different colors.
Continue reading “Roses Are Red and So Is . . . Blood?”NIGMS Grantees Receive National STEM Mentoring Award
In a previous post, we highlighted two NIGMS-funded winners of the 2018 Presidential Award for Excellence in Science, Mathematics and Engineering Mentoring (PAESMEM). For January’s National Mentoring Month, we tell you about other awardees: J.K. Haynes, Virginia Shepherd, and Maria da Graça H. Vicente.
Continue reading “NIGMS Grantees Receive National STEM Mentoring Award”How Three Physician Scientists Are Taking Strides to Improve Our Health
Brain injuries, cancer, infections, and wound healing are some of the complex and pressing health concerns we face today. Understanding the basic science behind these diseases and biological processes is the key to developing new treatments and improving patient outcomes. Physician scientists—medical doctors who also conduct laboratory research—are essential to turning knowledge gained in the lab into innovative treatments, surgical advances, and new diagnostic tools.
In this blog, we highlight the work and impact of three surgeon scientists funded by NIGMS at different stages in their careers: Dr. Nicole Gibran (current grantee), Dr. Rebecca Minter (former grantee), and Dr. Carrie Sims (former grantee). Their work, despite the historical underrepresentation of women in the physician scientist training community, has led to revolutionary surgical treatments, new therapeutics, better screening, and improved quality of life for patients.
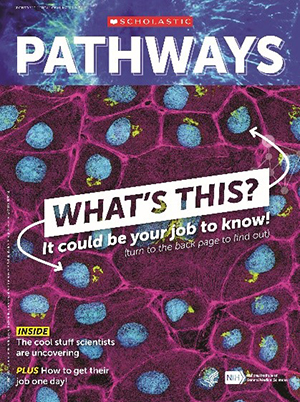
Continue reading “How Three Physician Scientists Are Taking Strides to Improve Our Health”Festive Flu Virus Structure
Credit: Rommie Amaro, Jacob Durrant, Adam Gardner, and colleagues.
Ah, December—a month suffused with light-filled holidays, presents, parties . . . and the spread of colds and flu. This playful image uses a festive approach to the serious science of understanding and finding ways to combat the flu virus.
Extreme Healing, Weird Genomics, and Bloodsucking Invaders
Quick quiz: Which organism . . .
- Can regrow a severed spinal cord?
- Is a culinary delicacy overseas but an invasive pest in the U.S.?
- Reveals insights about tissue regeneration, evolution, and cancer biology?
Continue reading “Extreme Healing, Weird Genomics, and Bloodsucking Invaders”
CRISPR Illustrated
You’ve probably heard news stories and other talk about CRISPR. If you’re not a scientist—well, even if you are—it can seem a bit complex. Here’s a brief recap of what it’s all about.
In 1987, scientists noticed weird, repeating sequences of DNA in bacteria. In 2002, the abbreviation CRISPR was coined to describe the genetic oddity. By 2006, it was clear that bacteria use CRISPR to defend themselves against viruses. By 2012, scientists realized that they could modify the bacterial strategy to create a gene-editing tool. Since then, CRISPR has been used in countless laboratory studies to understand basic biology and to study whether it’s possible to correct faulty genes that cause disease. Here’s an illustration of how the technique works.
Surgeon Chris McCulloh Stands Up to Disability

Credit: Chris McCulloh.
Chris McCulloh
Job: 4th-year general surgical resident, Morristown Medical Center in New Jersey
Grew up in: Manhattan
When not at work, he’s: Programming, coding, thinking about artificial intelligence, and machine learning
Hobbies: Writing/producing electronic music, weightlifting
Ten years ago, Chris McCulloh planned to enter medical school and fulfill his dream of becoming a surgeon. Instead, just months before he was to start med school, he ended up a patient. A freak accident—slipping on a hardwood floor, flying backwards, and landing neck-first on the edge of a glass coffee table—left him with both legs paralyzed at age 28. Undaunted, he deferred entering medical school for a year, undergoing surgery and spending months in rehab.

McCulloh prepares for surgery while “20/20” host Elizabeth Vargas stands alongside him as part of a 2017 interview.
Credit: Morristown Medical Center.
McCulloh has since finished medical school and recently completed a 2-year pediatric surgery research fellowship at Nationwide Children’s Hospital in Columbus, Ohio. He is now two-thirds of the way through his surgical residency at the Morristown (New Jersey) Medical Center, thanks to the assistance of a specialized wheelchair that allows him to stand nearly to his 6-foot-3 height and helps him perform five to six surgeries a day.
He’s received plenty of attention for being a surgeon with a disability. Along with several print media stories, he was interviewed in 2013 for CBS’ “The Doctors,” and in 2017, ABC’s “20/20” included McCulloh in an episode on physicians with disabilities. But it’s not the wheelchair that distinguishes McCulloh, says Gail Besner, a pediatric surgeon and researcher who hired McCulloh as a postdoctoral fellow. Rather, it’s his enthusiasm, natural research skills, and exceptional surgical prowess that make him special. Besner sees no reason why he won’t reach his goal of landing a highly competitive pediatric surgical residency. “I think he’s capable of doing anything he puts his mind to,” she says.
Continue reading “Surgeon Chris McCulloh Stands Up to Disability”